Reading Time: 5 minutes
Haemorrhoids
Summary: 30 Sec Read
Introduction:
- Haemorrhoids are swollen and inflamed blood vessels in the rectal and anal area.
- Common and uncomfortable condition causing pain and discomfort.
Overview:
- Two types: Internal (above dentate line) and External (painful, under the skin).
- Develop when blood vessels in the anal canal become swollen and inflamed.
Causes:
- Straining during bowel movements.
- Chronic constipation or diarrhea.
- Pregnancy.
- Obesity.
- Sedentary lifestyle.
- Low-fiber diet.
- Straining during lifting.
- Genetics.
Risk Factors:
- Age.
- Gender (more common in men).
- Pregnancy.
- Chronic constipation or diarrhea.
- Obesity.
Symptoms:
- Itching or irritation.
- Pain or discomfort (external).
- Bleeding.
- Prolapse (internal).
- Swelling and inflammation.
- Mucus discharge.
Complications of Untreated Haemorrhoids:
- Thrombosis (blood clots).
- Strangulation (loss of blood supply).
- Anemia (from chronic bleeding).
- Infection.
Diagnosis:
- Physical examination.
- Proctoscopy.
- Sigmoidoscopy (for lower colon examination).
Treatment Options:
- Medical interventions (creams, ointments, suppositories, wipes).
- Endoscopic procedures (rubber band ligation, sclerotherapy).
- Surgery (haemorrhoidectomy, stapler haemorrhoidopexy).
Prevention:
- High-fiber diet.
- Hydration.
- Regular exercise.
- Proper bathroom habits.
- Weight management.
When to Seek Medical Advice:
- Abdominal pain.
- Difficulty breathing.
- Rapid weight gain.
- Abdominal swelling.
- Fever or signs of infection.
Introduction
Haemorrhoids, commonly known as piles, are a prevalent and uncomfortable medical condition that affects millions of people worldwide. Characterized by swollen and inflamed blood vessels in the rectal and anal area, haemorrhoids can cause significant discomfort and pain. In this comprehensive blog article, we will delve into the causes, risk factors, symptoms, and potential complications of untreated haemorrhoids. We will also explore various diagnostic methods and available treatments, ranging from medical interventions to surgical procedures, as well as the importance of prevention and home care. Lastly, we will discuss when it’s crucial to seek medical advice for this condition.
Overview of Haemorrhoids
Haemorrhoids are vascular structures in the anal canal that aid in maintaining fecal continence. They consist of blood vessels, connective tissue, and a surrounding layer of smooth muscle. When these blood vessels become swollen and inflamed, they can lead to the development of haemorrhoids.
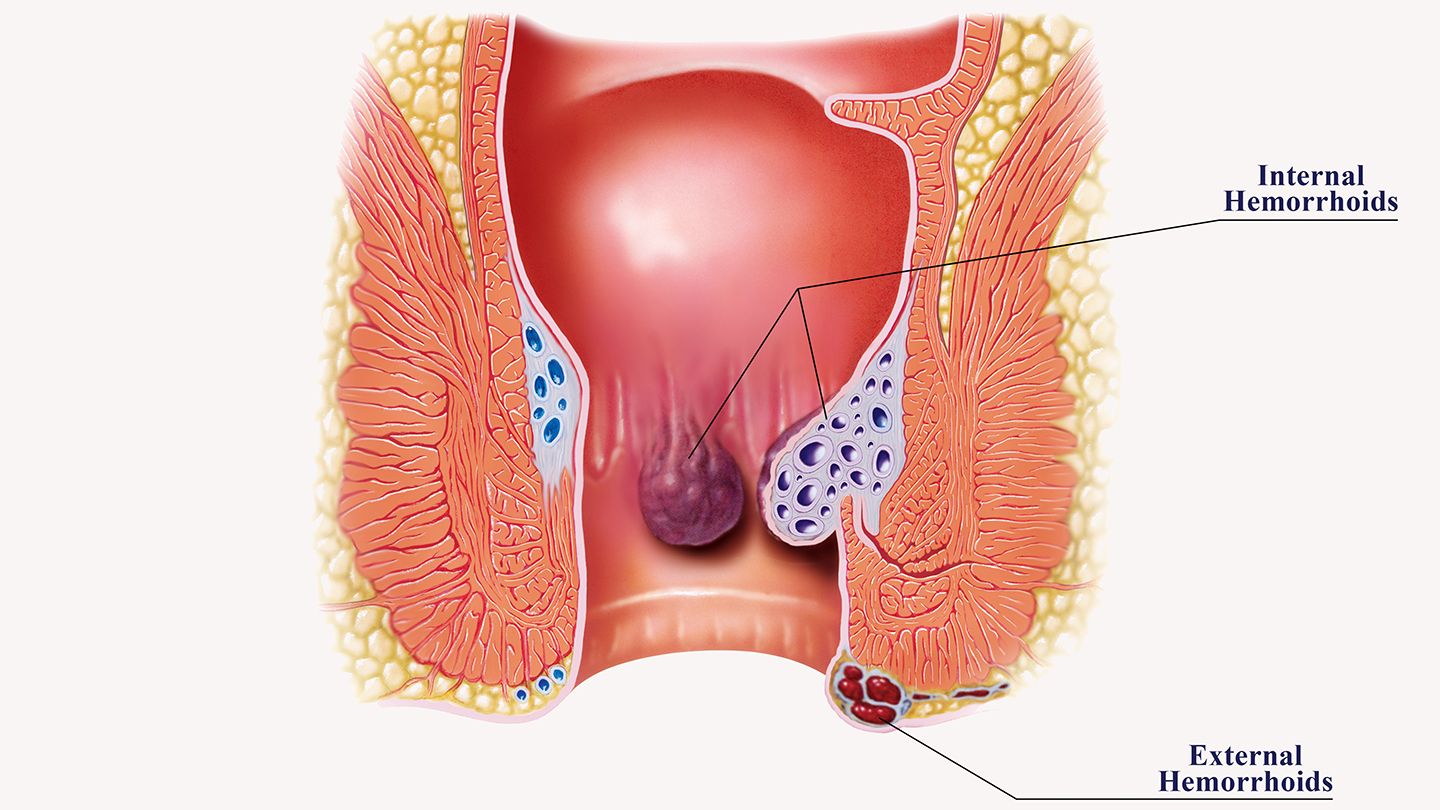
There are two types of haemorrhoids:
- Internal Haemorrhoids: These form inside the rectum and are usually painless because they are located above the dentate line, where pain receptors are absent. However, they may cause discomfort, bleeding, or prolapse, where they protrude outside the anus.
- External Haemorrhoids: These develop under the skin surrounding the anus and can be painful. They may cause itching, bleeding, and irritation.
Causes of Haemorrhoids
The precise cause of haemorrhoids is not always clear, but several factors contribute to their development:
- Straining during Bowel Movements: The most common cause is excessive straining during bowel movements, which can increase pressure in the anal and rectal area and lead to the development of haemorrhoids.
- Chronic Constipation or Diarrhea: Prolonged episodes of constipation or diarrhea can put significant pressure on the blood vessels in the anal area, leading to haemorrhoids.
- Pregnancy: Pregnant women are more susceptible to haemorrhoids due to increased pressure on the rectal veins caused by the growing uterus.
- Obesity: Being overweight or obese can contribute to haemorrhoid development due to increased pressure on the pelvic region.
- Sedentary Lifestyle: Lack of physical activity and prolonged sitting can also play a role in the formation of haemorrhoids.
- Low-Fiber Diet: A diet lacking in fiber can lead to constipation, which is a significant risk factor for haemorrhoids.
- Straining during Lifting: Lifting heavy objects with improper technique can strain the rectal area and contribute to haemorrhoid development.
- Genetics: Some individuals may have a genetic predisposition to developing haemorrhoids.
Risk Factors for Haemorrhoids
While haemorrhoids can affect anyone, certain factors increase the likelihood of their occurrence:
- Age: As people age, the tissues supporting the blood vessels in the rectal area may weaken, making haemorrhoids more likely.
- Gender: Men are more prone to developing haemorrhoids than women.
- Pregnancy: The increased pressure on the pelvic area during pregnancy raises the risk of haemorrhoids.
- Chronic Constipation or Diarrhea: People with recurrent constipation or diarrhea have a higher risk of developing haemorrhoids.
- Obesity: Being overweight or obese increases the pressure on the rectal veins, making haemorrhoids more likely.
Symptoms of Haemorrhoids
The symptoms of haemorrhoids can vary depending on their type and severity:
- Itching or Irritation: Piles may cause itching or irritation in the anal area.
- Pain or Discomfort: External haemorrhoids can be painful, especially during bowel movements.
- Bleeding: Bright red blood may be seen on toilet paper, in the toilet bowl, or coating the stool.
- Prolapse: Internal haemorrhoids may protrude outside the anus, leading to prolapse.
- Swelling and Inflammation: The anal area may appear swollen and red.
- Mucus Discharge: Some individuals may experience mucus discharge from the anus.
Complications of Untreated Haemorrhoids
If left untreated, haemorrhoids can lead to various complications:
- Thrombosis: External haemorrhoids may develop blood clots, causing severe pain and swelling.
- Strangulation: Prolapsed internal haemorrhoids may become trapped outside the anus and have their blood supply cut off, resulting in strangulated haemorrhoids.
- Anemia: Chronic bleeding from haemorrhoids can lead to iron deficiency anemia.
- Infection: In some cases, haemorrhoids can become infected, causing further complications.
Diagnosis of Haemorrhoids
To diagnose haemorrhoids, a medical professional will perform a physical examination of the rectal and anal area. They may use a gloved finger to feel for any abnormalities or perform a visual inspection.
In cases where internal haemorrhoids are suspected or if there are other concerns, the following diagnostic procedures may be performed:
- Proctoscopy: A proctoscope, a small tube with a light and camera, is inserted into the rectum to visualize the internal haemorrhoids and assess the extent of the condition.
- Sigmoidoscopy: This procedure allows doctors to examine the lower part of the colon and rectum for haemorrhoids or other abnormalities.
Treatment Options for Haemorrhoids
The treatment of haemorrhoids depends on their severity and the specific symptoms experienced. The following treatment options are available:
- Medical Interventions: Over-the-counter creams, ointments, and suppositories can provide relief from itching and discomfort. Medicated wipes may also be used to clean the anal area gently.
- Endoscopy: In some cases, endoscopic procedures may be used to address internal haemorrhoids. Techniques like rubber band ligation and sclerotherapy aim to reduce the blood flow to the haemorrhoid, causing it to shrink and eventually fall off.
- Surgery: When conservative treatments fail, or the haemorrhoids are particularly large or severe, surgical intervention may be necessary. Procedures like haemorrhoidectomy or hemorrhoid stapling are used to remove or reposition the haemorrhoids.
- Stapler Haemorrhoidopexy: This procedure, also known as PPH (Procedure for Prolapse and Haemorrhoids), is a less invasive surgical technique that staples the haemorrhoids in place, reducing blood flow and promoting their shrinkage.
Prevention of Haemorrhoids
Preventing haemorrhoids involves adopting healthy lifestyle habits and making some changes to your daily routine:
- High-Fiber Diet: Consuming a diet rich in fiber can help maintain regular bowel movements and prevent constipation.
- Hydration: Drinking plenty of water is essential to keep stools soft and prevent straining during bowel movements.
- Regular Exercise: Engaging in regular physical activity can improve bowel function and overall health.
- Proper Bathroom Habits: Avoid straining during bowel movements and do not delay going to the bathroom when you feel the urge.
- Weight Management: Maintaining a healthy weight reduces pressure on the pelvic area.
When to Seek Medical Advice
- Sudden and severe abdominal pain.
- Difficulty breathing.
- Rapid weight gain.
- Worsening abdominal swelling.
- Development of fever or signs of infection.
