कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Dr AvinashTank, is a super-specialist (MCh) Laparoscopic Gastro-intestinal Surgeon,
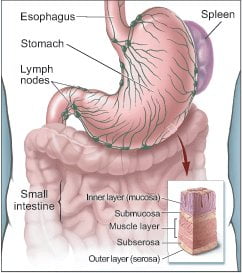
The stomach is a hollow organ in the upper abdomen, under the ribs.
It's part of the digestive system. Food moves from the mouth through the esophagus to the stomach. In the stomach, the food becomes liquid. Muscles in the stomach wall push the liquid into the small intestine.
The wall of the stomach has five layers:
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the stomach and other organs of the body.
Normal cells grow and divide to form new cells as the body needs them. When normal cells grow old or get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body doesn't need them, and old or damaged cells don't die as they should. The buildup of extra cells often forms a mass of tissue called a growth, polyp, or tumor.
Tumors in the stomach can be benign (not cancer) or malignant (cancer). Benign tumors are not as harmful as malignant tumors:
The stomach is a hollow organ in the upper abdomen, under the ribs.
It's part of the digestive system. Food moves from the mouth through the esophagus to the stomach. In the stomach, the food becomes liquid. Muscles in the stomach wall push the liquid into the small intestine.
The wall of the stomach has five layers:
When you're told that you have stomach cancer, it's natural to wonder what may have caused the disease. But no one knows the exact causes of stomach cancer. Doctors seldom know why one person develops stomach cancer and another doesn't.
Doctors do know that people with certain risk factors are more likely than others to develop stomach cancer. A risk factor is something that may increase the chance of getting a disease.
Studies have found the following risk factors for stomach cancer:
Studies suggest that people who eat a diet high in foods that are smoked, salted, or pickled have an increased risk for stomach cancer. On the other hand, people who eat a diet high in fresh fruits and vegetables may have a lower risk of this disease.
Most people who have known risk factors do not develop stomach cancer. For example, many people have an H. pylori infection but never develop cancer.
On the other hand, people who do develop the disease sometimes have no known risk factors.
Early stomach cancer often does not cause symptoms. As the cancer grows, the most common symptoms are:
Most often, these symptoms are not due to cancer. Other health problems, such as an ulcer or infection, can cause the same symptoms. Anyone who has these symptoms should tell their doctor so that problems can be diagnosed and treated as early as possible.
If you have symptoms that suggest stomach cancer, your doctor will check to see whether they are due to cancer or to some other cause. Your doctor may refer you to a gastroenterologist, a doctor whose specialty is diagnosing and treating digestive problems.
Your doctor will ask about your personal and family health history. You may have blood or other lab tests. You also may have:
If the biopsy shows that you have stomach cancer, your doctor needs to learn the stage (extent) of the disease to help you choose the best treatment.
Staging is a careful attempt to find out the following:
When stomach cancer spreads, cancer cells may be found in nearby lymph nodes, the liver, the pancreas, esophagus, intestine, or other organs. Your doctor may order blood tests and other tests to check these areas:
Sometimes staging is not complete until after surgery to remove the tumor and nearby lymph nodes.
When stomach cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if stomach cancer spreads to the liver, the cancer cells in the liver are actually stomach cancer cells. The disease is metastatic stomach cancer, not liver cancer. For that reason, it is treated as stomach cancer, not liver cancer. Doctors call the new tumor "distant" or metastatic disease.
These are the stages of stomach cancer:
The choice of treatment depends mainly on the size and location of the tumor, the stage of disease, and your general health.
Treatment for stomach cancer may involve surgery, chemotherapy, or radiation therapy. You'll probably receive more than one type of treatment. For example, chemotherapy may be given before or after surgery. It's often given at the same time as radiation therapy.
Your health care team can describe your treatment choices, the expected results, and the possible side effects. Because cancer therapy often damages healthy cells and tissues, side effects are common. Before treatment starts, ask your health care team about possible side effects, how to prevent or reduce these effects, and how treatment may change your normal activities. You and your health care team can work together to make a treatment plan that meets your needs.
The type of surgery for stomach cancer depends mainly on where the cancer is located. The surgeon may remove the whole stomach or only the part that has the cancer.
You and your surgeon can talk about the types of surgery and which may be right for you:
The time it takes to heal after surgery is different for each person, and you may be in the hospital for a week or longer. You may have pain for the first few days. Medicine can help control your pain. Before surgery, you should discuss the plan for pain relief with your doctor or nurse. After surgery, your doctor can adjust the plan if you need more pain relief.
Many people who have stomach surgery feel tired or weak for a while. Your health care team will watch for signs of bleeding, infection, or other problems that may require treatment.
The surgery can also cause constipation or diarrhea. These symptoms usually can be controlled with diet changes and medicine.
A cannula (hollow tube) is placed into the abdomen and abdomen will be inflated with carbon dioxide gas to create a space to operate. A laparoscope (a tiny telescope connected to a video camera) is put through one of the cannula which projects a video picture of the internal organs and appendix on a television monitor. Three cannulas are placed in different locations on your abdomen to allow surgeon to place instruments inside your belly to work and remove your appendix. After appendix is cut from all that it is connected to, it is placed inside a special bag & is pulled up into one of the incision and taken out.
Common advantages of laparoscopic appendectomy are: Less postoperative pain, shorten hospital stay, quicker return to bowel function, quicker return to normal activity & better cosmetic results
Most people with stomach cancer get chemotherapy. Chemotherapy uses drugs to kill cancer cells.
It may be given before or after surgery. After surgery, radiation therapy may be given along with chemotherapy.
The drugs that treat stomach cancer are usually given through a vein (intravenous). You'll probably receive a combination of drugs.
You may receive chemotherapy in an outpatient part of the hospital, at the doctor's office, or at home. Some people need to stay in the hospital during treatment.
Radiation therapy (also called radiotherapy) uses high-energy rays to kill cancer cells. It affects cells only in the part of the body that is treated. Radiation therapy is usually given with chemotherapy to treat stomach cancer.
The radiation comes from a large machine outside the body. You'll go to a hospital or clinic for treatment. Treatments are usually 5 days a week for several weeks.
Side effects depend mainly on the dose and type of radiation. External radiation therapy to the chest and abdomen may cause a sore throat, pain similar to heartburn, or pain in the stomach or the intestine. You may have nausea and diarrhea. Your health care team can give you medicines to prevent or control these problems.
It's common for the skin in the treated area to become red, dry, tender, and itchy.
in most cases, you will need some tests before your surgery. The tests routinely used include:
Our expert team of Anaesthetist will ask you questions pertaining to your health and to assess your fitness for surgery. You are requested to tell them in detail about your current and past medical ailments, allergic reactions you’ve had in the past and current medicines that you are taking like blood thinning medicine. This medicine should be stopped prior to surgery to minimize the risk of bleeding during /after surgery.
Anaesthesia is the use of drugs to make the body unable to feel pain for a period of time. General anaesthesia puts you into a deep sleep for the surgery. It is often started by having you breathe into a face mask or by putting a drug into a vein in your arm. Once you are asleep, an endotracheal or ET tube is put in your throat to make it easy for you to breathe. Your heart rate, breathing rate, and blood pressure (vital signs) will be closely watched during the surgery. A doctor watches you throughout the procedure and until you wake up. They also take out the ET tube when the operation is over. You will be taken to the recovery room to be watched closely while the effects of the drugs wear off. This may take hours. People waking up from general anaesthesia often feel “out of it” for some time. Things may seem hazy or dream-like for a while. Your throat may be sore for a while from the endotracheal (ET) tube.
Informed consent is one of the most important parts of “getting ready for surgery. It is a process during which you are told about all aspects of the treatment before you give written permission to perform the surgery.
Depending on the type of operation you have, there may be things you need to do to be ready for surgery:
Depending on your cancer type and stage, our goals for treatment are:
Surgery can be done for many reasons for treatment of cancer.
Curative Surgery
Diagnostic & Staging Surgery
Palliative Surgery
How surgery is performed? (Special surgery techniques): Open Or Laparoscopic
Open Surgery:
Laparoscopic Surgery
Biopsy is procedure to confirm the presence of cancer. It’s not essential before surgery. Usually biopsy is performed when 1. Suspicion is cause other than cancer, 2. When surgery cannot be done for cancer due to advanced stage of cancer or 3. Patient is unfit to undergo surgery. In these situation, biopsy guides for further therapy.
If all investigations suggest that cancer can be removed in totality from body, then biopsy can be avoided in to minimize the risk of spillage of cancer cell during biopsy procedure.
There is variety of way to perform biopsies:
Fine Needle Aspiration (FAN) biopsy
Core Needle biopsy
Excisional or Incisional biopsy
In most cases, you will need some tests before your surgery. The tests routinely used include:
Our expert team of Anaesthetist will ask you questions pertaining to your health and to assess your fitness for surgery. You are requested to tell them in detail about your current and past medical ailments, allergic reactions you’ve had in the past and current medicines that you are taking like blood thinning medicine. This medicine should be stopped 1 week prior to surgery.
Informed Consent
Informed consent is one of the most important parts of “getting ready for surgery”. It is a process during which you are told about all aspects of the treatment before you give your doctor written permission to do the surgery.
Depending on the type of operation you have, there may be things you need to do to be ready for surgery:
Anaesthesia is the use of drugs to make the body unable to feel pain for a period of time. General anaesthesia puts you into a deep sleep for the surgery. It is often started by having you breathe into a face mask or by putting a drug into a vein in your arm. Once you are asleep, an endotracheal or ET tube is put in your throat to make it easy for you to breathe. Your heart rate, breathing rate, and blood pressure (vital signs) will be closely watched during the surgery. A doctor watches you throughout the procedure and until you wake up. They also take out the ET tube when the operation is over. You will be taken to the recovery room to be watched closely while the effects of the drugs wear off. This may take hours. People waking up from general anaesthesia often feel “out of it” for some time. Things may seem hazy or dream-like for a while. Your throat may be sore for a while from the endotracheal (ET) tube.
You may feel pain at the site of surgery. We aim to keep you pain free after surgery with the help of latest and most effective technique or analgesic (pain relieving medicine).
As you are remains in bed on day of surgery, circulation of blood in leg become sluggish that may increase possibility of thrombo-embolism. To minimise it, you will be wearing leg stocking/ pneumatic compression boot to improve your leg circulation thus minimising the risk of thrombolism.
You may not feel much like eating or drinking, but this is an important part of the recovery process. Our health care team may start you out with ice chips or clear liquids. The stomach and intestines (digestive tract) is one of the last parts of the body to recover from the drugs used during surgery. You will need to have signs of stomach and bowel activity before you will be allowed to eat. You will likely be on a clear liquid diet until this happens. Once it does, you may get to try solid foods.
Once you are eating and walking, all tube/drains placed during surgery are removed, and then you may be ready to go home. Before leaving for home our health care team shall give you detailed guidance regarding diet, activities, medications & further plan of treatment.
There are risks that go with any type of medical procedure and surgery is no longer an exception. Success of surgery depends upon 3 factors: type of disease/surgery, experience of surgeon and overall health of patients. What’s important is whether the expected benefits outweigh the possible risks.
Doctors have been performing surgeries for a very long time. Advances in surgical techniques and our understanding of how to prevent infections have made modern surgery safer and less likely to damage healthy tissues than it has ever been. Still, there’s always a degree of risk involved, no matter how small. Different procedures have different kinds of risks and side effects. Be sure to discuss the details of your case with our health care team, who can give you a better idea about what your actual risks are. During surgery, possible complications during surgery may be caused by the surgery itself, the drugs used (anesthesia), or an underlying disease. Generally speaking, the more complex the surgery is the greater the risk. Complications in major surgical procedures include:

Experience
Award & Presentations
Satisfied Families
Successful Surgeries
Endoscopy
Laparoscopic Treatment of Crohn’s disease of Small Intestine. Dr Avinash Tank, Ahmedabad
Dr Avinash Tank, Dwarika Hospital, Ahmedabad October 15, 2022 7:06 pm
Low Hemoglobin, Constipation & Pain is due to Colon Crohn’s Colitis. Dr Avinash Tank, Ahmedabad
Dr Avinash Tank, Dwarika Hospital, Ahmedabad January 22, 2021 12:52 pm
Deleted video
Dr Avinash Tank, Dwarika Hospital, Ahmedabad November 9, 2023 12:53 pm
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Reading Time: 2 minutes Spread the love Mucus Discharge from Rectum After Stoma Surgery: Normal or Concerning? If you’ve had ostomy surgery, either a loop ileostomy…
Reading Time: 2 minutes Spread the love National Doctors Day 2024: Celebrating Our Medical Heroes on 1st July. Every year on 1st July, we come together…