कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Dr AvinashTank, is a super-specialist (MCh) Laparoscopic Gastro-intestinal Surgeon,
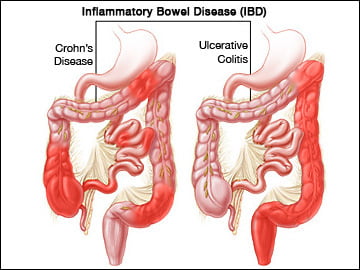
Ulcerative colitis is disease of large intestine. It causes ulceration and inflammation to large intestine (colon & rectum). Ulcerative colitis is a one part of inflammatory bowel disease (IBD). Crohn’s disease is another part of IBD. It’s a slowly progressive disease and it starts from below (rectum) and extend upwards to involve various parts of large intestine. It’s a chronic disease (i.e it persists for many years) so it need treatment/care for rest of the life. Available medicines keeps disease under control (remission) and disease may come back (recurrence) sometime after holding the medicines. Ulcerative colitis in most of the cases remains under control with medical treatment. But in few cases it can be uncontrollable with medicines and sometimes can lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission.
The exact cause of ulcerative colitis is unknown; genes, environment, and immune system all play a role. Smoking appears to be a protective effect against the development of ulcerative colitis, this is in contrast to Crohn's disease, which is more common in smokers and appears to be aggravated by the habit. Both ulcerative colitis and Crohn's disease are more common among women who use oral contraceptives. Patients who have had an appendectomy appear to be at increased risk for developing ulcerative colitis.
Ulcerative colitis and colonic Crohn's disease often have similar clinical presentations. Both may present with diarrhea and the passage of mucus. Patients with ulcerative colitis tend to have more urgency to pass stool as rectum is always affected by disease than those with Crohn's disease. Passage of blood in stool (rectal bleeding) is also common in ulcerative colitis. Abdominal pain is uncommon in ulcerative colitis. Its suggest either onset of complications of ulcerative colitis or Crohn’s disease.
Pain/pus discharge/fistula-in-ano are usually not seen with Ulcerative colitis and these symptoms are suggestive of Crohn’s disease. As Ulcerative colitis is a systemic (i.e., autoimmune) origin, patients may symptoms related to other organs in upto 5-25% cases.
The stomach is a hollow organ in the upper abdomen, under the ribs.
It's part of the digestive system. Food moves from the mouth through the esophagus to the stomach. In the stomach, the food becomes liquid. Muscles in the stomach wall push the liquid into the small intestine.
The wall of the stomach has five layers:

As symptoms of ulcerative colitis mimic other infective diseases (C. difficile, Entamoeba histolytica, C. jejuni, and Salmonella enteritidis) and Crohns disease, so proper diagnosis is essential. Each disease has different line of treatment. Stepwise tests are conducted to establish the proper diagnosis.
Blood tests: To check for anaemia & protein levels (due to blood loss) & to check for signs of infection.
Stool sample: White blood cells in your stool can indicate ulcerative colitis. A stool sample can also help rule out other disorders, such as infections caused by bacteria, viruses and parasites.
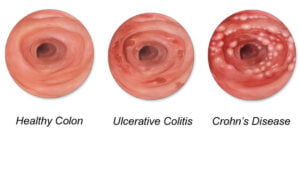
Both diseases, Ulcerative colitis (UC) and Crohn’s disease (CD), share many features but need to be differentiated as principal of treatment differs.


Medicine is first line of treatment. With medicines, the disease comes under control (remission) in most of patients. There is possibility that symptoms may not improve or worsen despite treatment, and then next line of treatment is started. Surgery is reserved for its complications. Severity of disease decides the line of treatment.
These drugs are normally reserved for people who haven’t responded well to other medications. Cyclosporine has the potential for serious side effects, such as kidney and liver damage, seizures, and fatal infections, and is not for long-term use.
They block the inflammatory response of the body and help reduce the inflammation in the colon. They may be used if other medicines don’t control your symptoms. These medicines are contra-indicated if there is any type on of infection in body like tuberculosis and active infections. These drugs also are associated with a small risk of developing certain cancers such as lymphoma and skin cancers.
Candidate for Surgery: Surgery is needed only if patient doesn’t responds to medical treatment and/or develop any of its complications like toxic megalcon, perforation, growth retardation in children.
Rational for Surgery: Surgery is the only treatment that offers chances of cure from disease as it removes the disease colon & rectum.

About the Surgery: Ideally whole rectum should be removed to get complete cure that need permanent stoma on tummy. New procedure known as Pouch surgery (resortive procto-colectomy), eliminate the need of permanent stoma thus improves the overall quality of life. This surgery is performed usually on two stages. In first stage, diseased colon and rectum is removed and new rectum is made from part of small intestine and then connected to lower end of rectum with the help of specialised instruments (stapler). Stool is diverted on tummy to facilitate the healing of new rectum and its connection with lower rectum. After surgery, the specific medical treatment of ulcerative colitis is not required, thus stopped. After about 2-3 months, temporary stoma of tummy is closed and stool is passed through normal passage. Stool frequency comes down significantly after surgery (2-3 times in day and 1-2 times at night) compared to 10-15 times stool frequency. These patients need regular meeting with doctor to watch their progress in health recovery.
In case of emergency surgery, only disease colon is removed. Pouch surgery is delayed till full recovery.

Experience
Award & Presentations
Satisfied Families
Successful Surgeries
Endoscopy
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Reading Time: 2 minutes Spread the love Mucus Discharge from Rectum After Stoma Surgery: Normal or Concerning? If you’ve had ostomy surgery, either a loop ileostomy…
Reading Time: 2 minutes Spread the love National Doctors Day 2024: Celebrating Our Medical Heroes on 1st July. Every year on 1st July, we come together…