कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Dr AvinashTank, is a super-specialist (MCh) Laparoscopic Gastro-intestinal Surgeon,
Portal hypertension is a high blood pressure in the portal blood system which is the portal vein and its branches, which drain from most of the intestines to the liver. If the vessels in the liver are blocked, blood cannot flow properly through the liver. As a result, high pressure in the portal system develops. This increased pressure in the portal vein over a time may lead to the development of large, swollen veins (varices) within the esophagus, stomach, rectum, or umbilical area (belly button). Varices can rupture and bleed, resulting in potentially life-threatening complications.
The blockage of blood vessels can happen at any of three places. One, Pre-hepatic i.e blockage of portal vein before it enters into the liver. Second, blockage inside the liver and Third, post-hepatic, blockage of blood vessels (hepatic veins) outside the liver. There are different causes of blockage at all three levels.
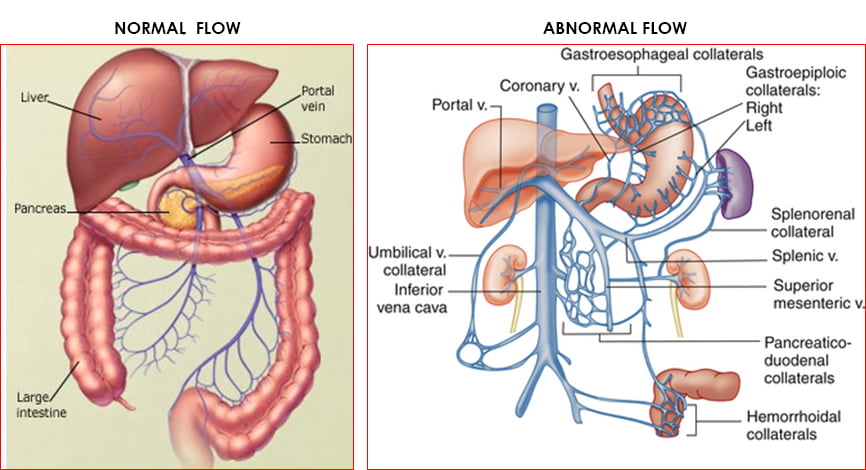
The most common cause of portal hypertension is cirrhosis of the liver. Cirrhosis is a condition in which the liver slowly deteriorates and is unable to function normally due to chronic, or long lasting, injury. Scar tissue replaces healthy liver tissue and partially blocks the flow of blood through the liver.
Other causes of portal hypertension include blood clots in the portal vein, blockages of the veins that carry the blood from the liver to the heart, a parasitic infection called schistosomiasis. Sometimes the cause is unknown despite all investigations.
Symptoms of portal hypertension are non-specific. Vague abdominal discomfort is common but non-specific. Usually portal hypertension is diagnosed when it progress to its complications. In vast majority of the cases, one of the complications may be the first clue about it.
The main symptoms and complications of portal hypertension include:
Based on symptoms, blood test, Sonography with Doppler study & Endoscopy is usually required to make diagnosis.
The portal hypertension itself is difficult to treat effectively, except by treating the underlying cause (where possible) and liver transplantation (if indicated and feasible).
Portal venous pressure can be reduced by medicine (beta-blockers ± nitrates) and by using surgery (shunt procedures) to create an new joint ( anastomosis) between the portal systemic veins.
Medicine
Endoscopic Therapy
Transjugular intrahepatic portosystemic shunt (TIPS)
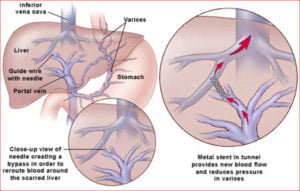
This is a radiological procedure, connecting the portal and hepatic veins using a stent. The purpose of a TIPS is to decompress the portal venous system, to prevent re-bleeding from varices or to reduce the formation of ascites. However, there are potential complications - hepatic encephalopathy and deteriorating liver function. The stent may stenose; it requires follow-up and may require repeat procedures.
Surgical porto-systemic shunts: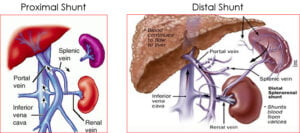
Devascularisation procedures:
This depends on the prognosis of the underlying disease, and on the outcome of any complications such as variceal bleeding.

Experience
Award & Presentations
Satisfied Families
Successful Surgeries
Reading Time: 5 minutes Spread the love कनकधारा स्तोत्र, धन प्राप्ति का चमत्कारी उपाय धन की तलाश में हम सभी अपने जीवन में एक समय…
Reading Time: 2 minutes Spread the love Mucus Discharge from Rectum After Stoma Surgery: Normal or Concerning? If you’ve had ostomy surgery, either a loop ileostomy…
Reading Time: 2 minutes Spread the love National Doctors Day 2024: Celebrating Our Medical Heroes on 1st July. Every year on 1st July, we come together…
Lorem Ipsum is simply dummy text of the printing and typesetting industry. Lorem Ipsum has been the industry's standard dummy text ever since the 1500s, when an unknown printer took a galley of type and scrambled it to make a type specimen book. It has survived not only five centuries, but also the leap into electronic typesetting, remaining essentially unchanged.